INTRODUCTION
Here’s a simplified and professional version of the guidance on when not to use naltrexone, with key terms emphasized:
Conditions That Preclude Naltrexone Use:
- Avoid naltrexone if you are currently taking opioid medications.
- Do not use if you have an opioid dependence.
- It is not suitable during acute opioid withdrawal or if you exhibit any withdrawal symptoms.
- Avoid if you have not passed a naloxone challenge test or if you test positive for opioids in a urine test.
- It should not be used if you have acute hepatitis or liver failure.
- Do not use if you are allergic or have had a hypersensitivity reaction to naltrexone, polylactide-co-glycolide (PLG), or any other components of the medication.
Inform your health care provider of any recent opioid use or history of opioid addiction before beginning naltrexone to prevent withdrawal symptoms. Your provider may conduct a naloxone challenge test and require a urine test for opioids before starting treatment.
Understanding Naltrexone and Its Uses:
Naltrexone is a medication primarily used to manage opioid use disorder (OUD) and alcohol use disorder. It is an opiate antagonist, meaning it blocks the euphoric effects caused by opioids and alcohol, which can help prevent the urge to use these substances. Importantly, naltrexone does not induce the ‘high’ associated with narcotics, nor does it lead to dependency.
This medication is offered in two forms: as a long-acting intramuscular injection under the brand name Vivitrol, and as a 50 mg oral tablet available generically.
Treatment with naltrexone begins only after full detoxification from opioids, ensuring the individual is not dependent. Starting naltrexone while opioids are still in the body can trigger severe withdrawal symptoms.
It’s essential not to commence naltrexone therapy until completing a medically supervised withdrawal from opioids, which should last between 7 to 14 days to effectively prevent withdrawal complications that might necessitate hospitalization. If the patient has been taking longer-acting opioids like methadone or buprenorphine, an extended detox period may be necessary.
Key Guidelines for Naltrexone Users:
When taking naltrexone, it’s critical to avoid:
- All opioids, such as heroin, morphine, codeine, oxycodone, tramadol, and hydrocodone, whether they are prescribed or obtained illegally.
- Illicit drugs.
- Alcohol consumption.
- Central nervous system (CNS) depressants, including sedatives and tranquilizers, among others.
Attempting to use opioids in small amounts while on naltrexone is ineffective because the medication blocks the euphoric and sedative effects, preventing any ‘high’. Trying to overcome this block with larger doses of opioids is extremely dangerous and can result in severe consequences, including overdose, coma, or death. After ceasing opioid use, your sensitivity to opioids increases, making even small doses hazardous.
Handling Missed Doses of Naltrexone:
It’s important not to skip any doses of naltrexone as prescribed. While on naltrexone, your tolerance to opioids decreases, and returning to your previous opioid doses can be extremely dangerous, possibly resulting in severe respiratory depression, circulatory collapse, or even death. The risk of a fatal overdose increases significantly towards the end of a dosing interval, after a missed dose, or upon discontinuation of treatment.
If you forget to take your oral naltrexone tablet, take it as soon as you remember. However, if it’s nearly time for your next scheduled dose, skip the one you missed. Do not take an extra tablet to compensate for the missed dose.
Should you miss an appointment for your naltrexone injection, contact your healthcare provider immediately to arrange another appointment as soon as possible.
Guidelines for Managing Naltrexone Dosage:
Always follow your doctor’s instructions when taking naltrexone. Consuming more than the recommended dose, particularly over 50 mg in a single oral intake, significantly raises the risk of liver damage.

Naltrexone does not produce euphoria or a “high,” and it is generally not misused for such effects. However, excessive amounts can lead to serious liver (hepatic) injury. If you experience symptoms such as stomach pain, white stools, dark urine, or yellowing of the eyes—these are indicators of liver damage and require immediate medical attention.
Individuals with acute hepatitis or severe liver disease should avoid naltrexone. Additionally, it is not advisable for those currently using opioids or for individuals with certain liver conditions who depend on opioids for pain management.
Never share or sell naltrexone to others, particularly to those who are opioid users, as it can precipitate severe withdrawal symptoms.
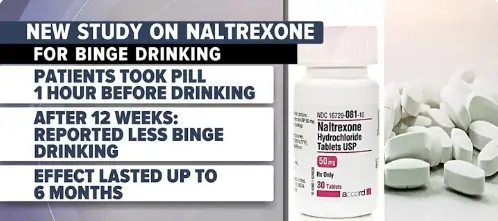
Naltrexone’s Role in Treating Alcohol Dependence
Naltrexone helps manage alcohol dependence by blocking the euphoric effects and sensations of intoxication that alcohol provides. This action helps individuals with alcohol use disorder (AUD) decrease their drinking, stay engaged in treatment, prevent relapses, and adhere to their medication plans.
However, it’s important to note that naltrexone does not stop the physical impairment caused by alcohol consumption. Therefore, you should not use naltrexone to enable driving or performing other tasks while under the influence of alcohol.
For effective treatment of alcohol dependence, you should not be actively drinking when you begin naltrexone therapy. Ideally, you should be capable of abstaining from alcohol in everyday environments like home and work before starting the medication.
Treatment with naltrexone should be part of a comprehensive program that includes counseling, support groups, and other behavioral therapies as recommended by your healthcare provider, applicable to both alcohol and opioid use disorders.
Eligibility for Naltrexone Treatment
Naltrexone is approved for adults aged 18 and older. Its safety and effectiveness in individuals younger than 18 have not been established by the FDA, and it is not recommended for this age group.
Prescription and Administration:
Naltrexone is available in both tablet and injectable forms. Tablets can be taken with or without food, though taking them with food may reduce stomach side effects. The injectable form, known as Vivitrol, is administered by a healthcare provider and must be given in a medical setting.
Warnings and Precautions:
Do not attempt to administer the injection yourself. Injectable naltrexone can cause serious problems at the injection site, including intense pain, blisters, hardening of the area, open wounds, significant swelling, dark scabs, and lumps. Report any of these symptoms to your healthcare provider immediately.
Health Conditions to Discuss:
Inform your doctor if you have kidney disease, bleeding disorders, low blood platelets, or lung conditions, as these may require additional precautions. If you have a history of depression, suicidal behavior, or other mental health issues, discuss these with your doctor before starting treatment. It’s important to alert family or close associates that you are using naltrexone, so they can monitor for signs of depression.
Operating Vehicles and Machinery:
Naltrexone may cause dizziness or drowsiness, impacting your ability to drive or operate machinery safely. Avoid these activities if you experience such side effects.
Allergies and Sensitivities:
You should not take naltrexone if you are allergic to it or any of its ingredients. Always inform your doctor about any past allergic reactions to medications.
Pregnancy and Breastfeeding:
If you are pregnant, planning to become pregnant, or breastfeeding, discuss your situation with your healthcare provider before starting naltrexone.
Distinguishing Naltrexone from Naloxone
Naltrexone vs. Naloxone:
It is crucial not to confuse naltrexone with naloxone (brand names include Narcan, Evzio). While both are related to opioid treatment, they serve different purposes. Naloxone is specifically used for emergency opioid overdose situations to reverse life-threatening effects such as respiratory depression.
Drug Interactions with Naltrexone:
Naltrexone may interact with a variety of substances. Before starting any new prescriptions, over-the-counter medications, vitamins, or supplements, it’s essential to consult with your doctor or pharmacist for a drug interaction review. While on naltrexone, opioid-containing medications for cough, colds, or diarrhea will not be effective. Non-narcotic alternatives should be used for managing pain, coughs, or diarrhea, and your healthcare provider can advise on the safest options.
Naltrexone Identification Card:
Carrying a naltrexone identification card at all times is recommended. This card informs medical personnel that you are undergoing naltrexone therapy, which is crucial in an emergency. You can obtain this card from your doctor, ensuring that you receive appropriate care when needed.
If you experience symptoms like difficulty breathing, shortness of breath, coughing, or wheezing, which could suggest an allergic-type reaction similar to pneumonia, immediately contact your physician.
Essential Guidelines for Naltrexone Use
Safety Precautions with Naltrexone:
It is imperative not to use any opiates, such as heroin or other prescription or illicit opioids, while on naltrexone. Combining these substances with naltrexone can dramatically increase the risk of overdose, coma, and even death.
Conditions for Starting Naltrexone:
Do not start naltrexone if you are currently dependent on opioids or are experiencing withdrawal symptoms. You must first complete a medically-supervised opioid detoxification, which typically lasts between 7 to 14 days.
Important Pre-Treatment Discussions:
Inform your doctor about any recent opioid usage or a history of opioid dependence before beginning naltrexone. This is crucial to prevent severe withdrawal symptoms that might necessitate hospitalization.
Further Information:
This overview does not cover all the details needed for the safe and effective use of naltrexone. Ensure to read the complete prescribing information and discuss any questions or concerns with your healthcare provider.
FAQS
Should naltrexone be taken with food?
Yes, taking naltrexone tablets with food or after a meal can help reduce stomach side effects like nausea or pain.
How can side effects of naltrexone be reduced?
To minimize side effects like nausea when starting naltrexone, it is advisable to abstain from alcohol for at least 3 to 7 days before beginning treatment.
What should not be taken with naltrexone?
Individuals on naltrexone must avoid all opioids (such as heroin, morphine, codeine, oxycodone, tramadol, hydrocodone, and other legal or illegal opioids), illicit drugs, alcohol, and CNS depressants like sedatives and tranquilizers.
How often can you take naltrexone?
Adults can take 50 mg of naltrexone (one tablet) once daily if no withdrawal side effects occur. The appropriate use and dosage for children must be determined by a healthcare provider.
When does naltrexone start working?
Oral naltrexone begins to work within one hour of ingestion, making it effective quickly for treating opioid and alcohol use disorders. The intramuscular, extended-release form of naltrexone has two peak times: initially at about 2 hours after injection and then again 2 to 3 days later.
